Experts warn that antimicrobial resistance (AMR) is responsible for unprecedented child mortality rates, particularly in Africa and South East Asia, and call for urgent public health actions.
Alarming Rise in Child Deaths Linked to Antibiotic Resistance

Alarming Rise in Child Deaths Linked to Antibiotic Resistance
A recent study reveals that over three million children died from drug-resistant infections in 2022, highlighting a growing public health crisis.
Article text:
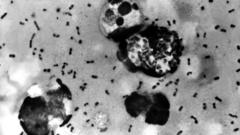
In a troubling revelation, a new study has indicated that over three million children across the globe lost their lives in 2022 due to infections resistant to antibiotics. The research, conducted by distinguished child health experts, particularly highlights the heightened risk faced by children in regions like Africa and South East Asia. Antimicrobial resistance (AMR), a condition where bacteria evolve and become unresponsive to standard antibiotic treatments, is becoming recognized as a significant public health crisis.
Utilizing data compiled from esteemed organizations such as the World Health Organization (WHO) and the World Bank, the study provides alarming insights into the impact of AMR on young lives. The findings underscore a stark more than tenfold increase in child deaths linked to resistant infections over the last three years, a situation exacerbated by the disruptions caused by the Covid-19 pandemic.
Antibiotics, crucial for treating a variety of bacterial infections—from skin issues to pneumonia—are facing resistance as their overuse and misuse become rampant. While antibiotics are ineffectual against viral infections such as colds and the flu, certain bacteria are developing resistance to commonly prescribed drugs. Furthermore, the development of new antibiotics has seen a decline, contributing to the crisis.
The report's lead authors, Dr. Yanhong Jessika Hu from the Murdoch Children's Research Institute in Australia and Professor Herb Harwell from the Clinton Health Access Initiative, noted with concern the sharp surge in the prescription of antibiotics classified as "watch" and "reserve"—both reserved for serious infections. Between 2019 and 2021, the utilization of "watch antibiotics" surged by 160% in South East Asia and 126% in Africa, while "reserve antibiotics" saw increases of 45% and 125% in these respective areas.
The authors caution that if bacterial resistance continues to escalate, treatment options for severe multidrug-resistant infections could virtually vanish. As Professor Harwell prepares to present these findings at the Congress of the European Society of Clinical Microbiology and Infectious Diseases in Vienna, he emphasizes the widespread impact of AMR, particularly on vulnerable populations.
While the WHO has flagged AMR as a dire global health concern, experts like Professor Harwell assert that tackling this issue requires multifaceted solutions that are not easily implemented. He emphasizes preventive measures, advocating for enhanced immunization, improved sanitation, and effective hygiene practices to stave off resistant infections.
Dr. Lindsey Edwards, a microbiology lecturer at King’s College London, has described the findings as critical, manifesting an alarming trend compared to earlier statistics. This should serve as a pressing alert to global health leaders, as unchecked AMR threatens to reverse the significant advances made in child health, especially in at-risk regions.
In a troubling revelation, a new study has indicated that over three million children across the globe lost their lives in 2022 due to infections resistant to antibiotics. The research, conducted by distinguished child health experts, particularly highlights the heightened risk faced by children in regions like Africa and South East Asia. Antimicrobial resistance (AMR), a condition where bacteria evolve and become unresponsive to standard antibiotic treatments, is becoming recognized as a significant public health crisis.
Utilizing data compiled from esteemed organizations such as the World Health Organization (WHO) and the World Bank, the study provides alarming insights into the impact of AMR on young lives. The findings underscore a stark more than tenfold increase in child deaths linked to resistant infections over the last three years, a situation exacerbated by the disruptions caused by the Covid-19 pandemic.
Antibiotics, crucial for treating a variety of bacterial infections—from skin issues to pneumonia—are facing resistance as their overuse and misuse become rampant. While antibiotics are ineffectual against viral infections such as colds and the flu, certain bacteria are developing resistance to commonly prescribed drugs. Furthermore, the development of new antibiotics has seen a decline, contributing to the crisis.
The report's lead authors, Dr. Yanhong Jessika Hu from the Murdoch Children's Research Institute in Australia and Professor Herb Harwell from the Clinton Health Access Initiative, noted with concern the sharp surge in the prescription of antibiotics classified as "watch" and "reserve"—both reserved for serious infections. Between 2019 and 2021, the utilization of "watch antibiotics" surged by 160% in South East Asia and 126% in Africa, while "reserve antibiotics" saw increases of 45% and 125% in these respective areas.
The authors caution that if bacterial resistance continues to escalate, treatment options for severe multidrug-resistant infections could virtually vanish. As Professor Harwell prepares to present these findings at the Congress of the European Society of Clinical Microbiology and Infectious Diseases in Vienna, he emphasizes the widespread impact of AMR, particularly on vulnerable populations.
While the WHO has flagged AMR as a dire global health concern, experts like Professor Harwell assert that tackling this issue requires multifaceted solutions that are not easily implemented. He emphasizes preventive measures, advocating for enhanced immunization, improved sanitation, and effective hygiene practices to stave off resistant infections.
Dr. Lindsey Edwards, a microbiology lecturer at King’s College London, has described the findings as critical, manifesting an alarming trend compared to earlier statistics. This should serve as a pressing alert to global health leaders, as unchecked AMR threatens to reverse the significant advances made in child health, especially in at-risk regions.